45 year female with SOB and anasarca
I've been given these three cases data here
https://alekyatummala.blogspot.com/2020/09/45-yr-female-with-anasarca.html?m=1
This may develop my competency in
a) reading and comprehending clinical data related to the case including history, clinical findings, investigations
b) come up with a diagnosis such as:
1) Anatomical location of the root cause
2) Physiological functional disability
3) Biochemical abnormalities that could be a root cause at a molecular level
4) Pathology that could reflect the root cause at a cellular level
c) a treatment plan for each of these patients of paraparesis that can have a pharmacological and non pharmacological component.
And
d) learning the scientific basis of diagnostic and therapeutic approach in terms of past collective experiences and experiments (aka evidence based medicine)
The first step to developing these competencies after reading and comprehending each patient data will be to
a) create a problem list for each patient in order of the patient's perceived priority
b) Discuss the root causes for the problem as described above in terms of anatomy, biochemistry and pathology, microbiology
and
c) discuss possible solutions to tackle these root causes from upstream (soil from which the roots begin) or downstream (to treating the stem and branches aka palliation) in terms of pharmacological (medicinal) and non pharmacological (such as prosthetics, implants) both in historical terms (past dominant treatments for the same cause and it's current evolution) as well as recent advances ( ongoing trials and innovative approaches even at a hypothetical stage).
1) What is your complete anatomic and etiologic diagnosis from the data available in the patient's online record linked above? (ignore the provisional diagnosis on admission mentioned in the case report)
Anatomic diagnosis: acute kidney injury at glomerulus, kimmelstein Winston lesions could be a possibility in a pathologic view where there is mesangial thickning there could be other causes also.
Reference: Robbins pathologic basis of disease pg 1111
Etiologic diagnosis:
diabetic nephropathy
Nephrotic syndrome
2) What are the reasons for her:
Azotemia
A reduction in GFR causes reduced excretion of nitrogenous wastes leading to azothemia blood urea nitrogen more than 20mg/ dl, urea more than 40 mg/dl
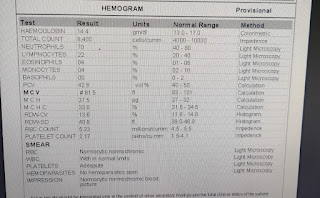
Anemia
there is kidney injury there is reduction in erythropoietin production which leads to anaemia due to erythroid hypoplasia
Hypoalbuminemia
Increased glomerular capillary permeability due to
Acidosis
reduction in GFR leads to reduced H+, and other organic acids excretion leading to acidosis. metabolic acidosis increased anion gap
3) What was the rationale for her treatment plan detailed day wise in the record?
Day 1
HCO3 was given to treat acidosis - target HCO3 22meq/l
potassium was given to counteract hypookalemia
Day 2
insulin was given to correct hyperglycemia
pantoprazole was given to prevent curling ulcer
Vitamin B9 or Folic Acid, iron was given to reat anaemia
furocemide was given to reuce fluid overload (evidenced by pulmonary edema)
Day 3
furcemide - reduce fluid overload
spirinolactone - reduce potasium loss from furocemide
Vitamin B9 or Folic Acid, iron was given to reat anaemia
nicardipine - to achieve target BP of 130/80
eruthropoietin to treart underlying cause of anaemia
calcium and vitamin d3 - reuce renal osteodystrophy
tab sodium bicarbonate - reduce/prevent metabolic acidosis
potassium was given to counteract hypookalemia
renal replacement therapy
Day 5
lactulose to reduce encephalopathy
protien to counteract protien loss
ceftrioxone to prevent infection as a risk of renal replacement therapy
Particularly mention rationale and efficacy for some of the drugs administered such as oral and iv bicarbonate? When is iv or oral bicarbonate indicated and why is it contraindicated in certain situations?
Metabolic acidosis in patients with chronic kidney disease: Oral (off-label): Note: KDIGO guidelines suggest oral replacement when plasma HCO3- concentrations are <22 mEq/L (KDIGO 2013).
Initial: 15.4 to 23.1 mEq/day in divided doses (eg, 650 mg tablet 2 to 3 times daily); titrate to normal serum bicarbonate concentrations (eg, 23 to 29 mEq/L) or up to 5850 mg/day; baking soda may be used as an alternative in patients who cannot take tablets (Chen 2014; KDIGO 2013; Kovesdy 2009; Raphael 2016). Avoid exceeding serum bicarbonate concentrations >32 mEq/L since this has been associated with increased mortality in patients with CKD (Navaneethan 2011).
https://reference.medscape.com/drug/sodium-bicarbonate-342305
4) What was the indication for dialysing her and what was the crucial factor that led to the decision to dialyze her on the third day of admission?
"Intractable dependent oedema resistant to diuretics
Pulmonary oedema
Severe hypertension
Potassium resistant to dietary control and medical intervention
Uraemic syndrome including anorexia, nausea, lethargy etc. (generally not until eGFR < 10 mL/min/1.73 m2)
Chronic acidosis resistant to bicarbonate therapy
Intractable anaemia despite erythropoietin and iron
Hyperphosphataemia despite binders"
Reference: davidson 23rd edition table 15.35
Indication in this case
severe shortness of breath - pulmonary edema
metabolic acidosis and refractory anuria
5) What are the other factors other than diabetes and hypertension that led to her current condition?
Failure of secondary prevention that is failure to seak medical help in eary stage of disease
6) What are the expected outcomes in this patient? Compare the outcomes of similar patients globally and share your summary with reference links.
kaplan - Meier survival rate of diabetic CKD is 37%,
5year survival is 40%
diabetes, low serum albumin, low socioeconomic status of this patient predict poor prognosis
FGF-23 levels is a novel marker for mortality
7) How and when would you evaluate her further for cardio renal HFpEF and what are the mechanisms of HFpEF in diabetic renal failure patients?
"The complications of CKD result in increased cardiac workload due to hypertension, volume overload, and anemia. Patients with CKD may also have accelerated rates of atherosclerosis and vascular calcification resulting in vessel stiffness."
these factors contribute to development left ventricular hypertrophy and left ventricular failure
Reference: CMDT 2020, topic on chronic kidney disease.
Frequency of echocardiography
at time of starting od renal replacement therapy
after 1 month of starting renal replacement therapy
after 3 months of starting or renal replacement therapy
then annually after starting of renal replacement therapy
any time if patient's symptoms change
reference: https://pubmed.ncbi.nlm.nih.gov/15806502/
8) What are the efficacies over placebo for the available therapeutic options being provided to her for her anemia?
"There was an improvement in haemoglobin (MD 1.90 gm/L, 95% CI -2.34 to -1.47) and haematocrit (MD 9.85%, 95% CI 8.35 to 11.34) with treatment and a decrease in the number of patients requiring blood transfusions (RR 0.32, 95% CI 0.12 to 0.83)."
ref: https://pubmed.ncbi.nlm.nih.gov/26790135/
9) What is the utility of tools like the CKD-AQ that assess the frequency, severity, and impact on daily activities of symptoms of anemia of CKD? Is Telugu among the 68 languages in which it is translated?
There are many studies which prove questionares efficatious and lead to early recognition of symptoms and prompt treatment.
https://doi.org/10.1016/j.jval.2018.09.2321
10) What is the contribution of protein energy malnutrition to her severe hypoalbuminemia? What is the utility of tools such as SGA subjective global assessment in the evaluation of malnutrition in CRF patients?
"subjective global assessment can be used effectively by providers from different disciplines, such as nursing, dietitians, and physicians; and in some studies has beenfound to be reproducible, valid, and reliable."
reference:
2) A similar patient data as above with diabetes and renal failure with metabolic acidosis and hypoalbuminemia logged by intern Dr Bhavya here
https://bhavyayammanuru.blogspot.com/2020/09/aki-secondary-to-uti.html?m=1
Please comment on the differences in the diagnosis, therapy and outcomes in both these two patients.
case 1: chronic kidney disease
The aims of management in CKD are to:
• monitor renal function
• prevent or slow further renal damage
• limit complications of renal failure
• treat risk factors for cardiovascular disease
• prepare for RRT, if appropriate
Case 2: acute kidney injury
•fluid status
If hypovolaemic: optimise systemic haemodynamic statu
If fluid-overloaded, prescribe diuretic
•correct hyperkalaemia if K+ > 6.5 mmol/L
•correct acidosis if H+ is > 100 nmol/L (pH < 7.0) - administer bicarbonate
• Discontinue potentially nephrotoxic drugs and reduce doses of therapeutic drugs
• nutritional support
•proton pump inhibitors to reduce curling ulcers
• Screen for infections and treat
• In case of urinary tract obstruction, drain lower or upper urinary tract as necessary
Would you agree with the provisional diagnosis shared for this 58 M in the online case report linked above?
yes, there was no symptoms suggesting of pre renal AKI like Volume depletion (vomiting, diarrhoea, burns, haemorrhage) Drugs (diuretics, ACE inhibitors, ARBs, NSAIDs, iodinated contrast) Liver disease
and symptoms like "Decreased urinary stream since 3days not passing urine since 1 day Pain abdomen since 1day." suggest a post renal AKI
What are the findings in the ultrasound of both kidneys? How do you explain those findings? Would it explain the etiology for his renal failure?
It is normal in size
corticomedullary differentiation normal
pelvi calyceal saperation normal
in pre renal aki there is less perfusion to kidney and kidney is structurally normal
doppler imaging would help in confirming less perfusion
loss of cortico medullary differintation is seen in CKD which helps in rulling out the condition
pelvi calyceal sustem is dilated in post renal AKI which helps in rulling out the condition

Comments
Post a Comment